This leaflet tells you about cervical screening.It aims to help you choose whether or not to have a cervical smear taken.
The human papilloma-virus (HPV) is a very common infection and most women get it at some time in their life. There are many types of HPV, and some types can cause abnormalities in the cervix. In some cases these abnormalities may, if left untreated, go on to develop into cervical cancer. Not all abnormalities develop into cancer however, and in many cases HPV clears up by itself.
HPV is easily transmitted during intimate sexual contact between partners. This includes intimate contact between men and women, and between partners of the same sex. The virus shows no symptoms. This means you or a partner could have had the virus for many months or years or from a previous relationship, without knowing it.
Cervical cancer can often be prevented. The signs that it may develop can be spotted early on so it can be stopped before it even gets started. Around 1400 women die of cervical cancer in Mumbai each year. However many of those who develop it have not been screened regularly. Not going for cervical screening is one of the biggest risk factors for developing cervical cancer.
A doctor will carry out your test. If you would prefer to see a female member of staff, please ask when you make your appointment.
We will ask you to undress from the waist down.
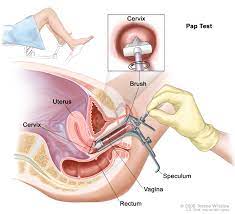
The doctor or nurse will ask you to lie down on a couch. They will then gently put a small instrument, called a speculum, into your vagina to hold it open. Then, they will wipe a small brush-like device over the cervix to pick up some cells. They will put these cells into a small container of liquid, and send it away for the cells to be transferred onto a slide and examined under a microscope. The test takes just a few minutes.
You might experience some discomfort or pain – try to relax by taking slow, deep breaths as it may hurt more if you are tense. If it is painful, tell the doctor straightaway as they may be able to reduce your discomfort.
HPV can cause abnormal changes in the cervix. If your screening result shows borderline cell changes or mild abnormalities (known as mild or low-grade dyskaryosis), an HPV test may be carried out on the sample of your cells taken during screening. This will help us decide if you need any further investigation, or if you can simply go back to routine screening in three or five years’ time (depending on your age).
You should not be tested during your period so try to make sure you get an appointment before or after your period is due. The best time is in the middle of your cycle.
If you use a spermicide, a barrier method of contraception, or a lubricant jelly, you should not use these for 24 hours before the test as the chemicals they contain may affect the test.
When you have the test, the doctor will tell you approximately when you will get your results.
If you have a screening result showing borderline cell changes or mild abnormalities, then your screening sample may be tested for HPV. If your sample is tested for HPV, then you will get this result at the same time as your screening result.
If you have a screening result showing borderline cell changes or mild abnormalities, then your screening sample may be tested for HPV. If your sample is tested for HPV, then you will get this result at the same time as your screening result.
This usually means that your sample did not show up clearly, so we need to take another one. This is called an ‘inadequate result’. On the other hand, screening may have found some small changes in the cells of the cervix. If abnormal changes (known as dyskaryosis) are detected, you will have what is called an ‘abnormal result’. If you have borderline or mild changes found at screening, you may be asked to come back again after six months for a repeat test. This is routine for any woman with borderline or mild changes if their screening sample hasn’t been tested for HPV. Your results letter will let you know if you need to come back for another screening test.
Yes. Your doctor will explain what needs to be done. They may simply ask you to come back for more cervical screening tests, because the abnormal cells may return to normal by themselves. However, they may ask you to go to hospital for a closer examination which is called ‘colposcopy’.
Yes. Regular cervical screening is the best way to detect changes to the cervix before cancer develops. Early detection and treatment can prevent cancer developing in around 75% of cases. Screening can also find cervical cancer early on, when treatment is more likely to be effective.
The laboratory that looks at your sample will keep it for at least 10 years. They can then compare your latest result with the ones you have had before. This is to make sure that you get any treatment you may need. They may review all screening records, including your sample, as part of our aim to offer a quality service and to help increase the expertise of specialist staff.
Copyright ©2021 Dr. Vrunda Karanjgaokar